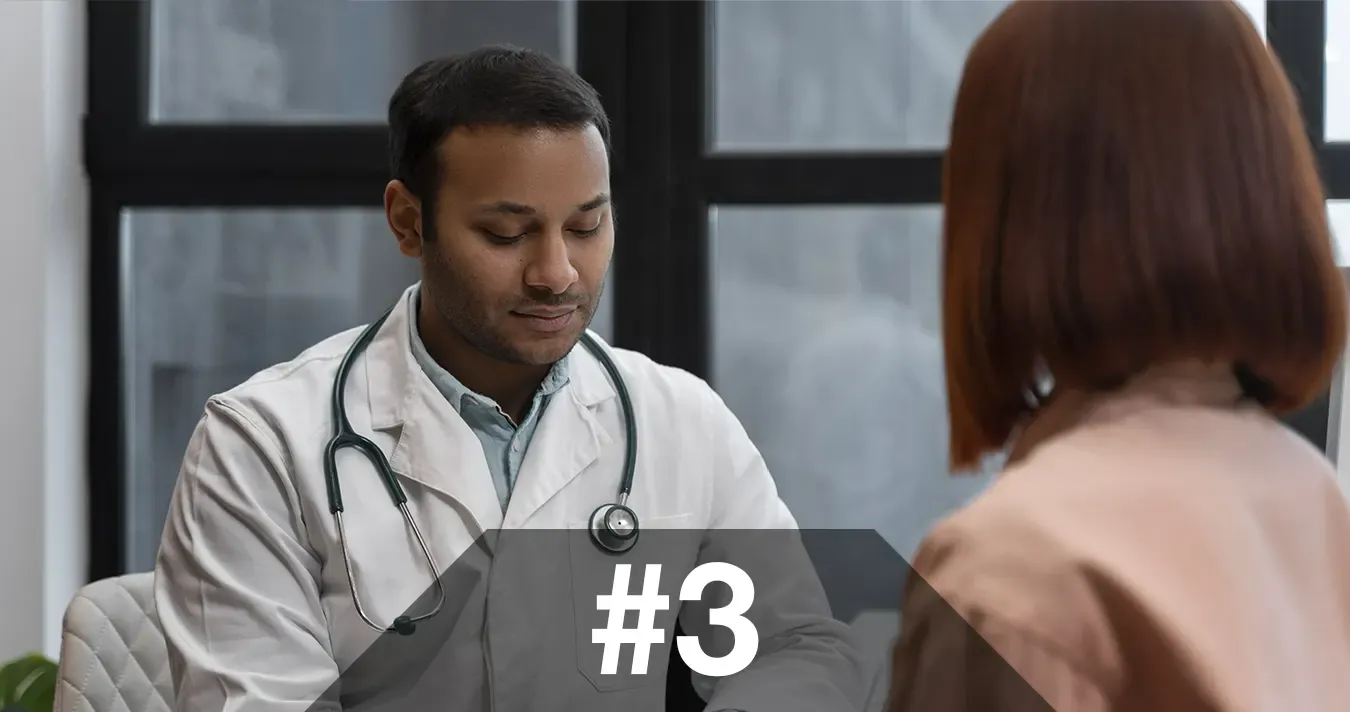
Clinical handovers involve the exchange of information between healthcare providers about a patient. Some examples of when clinical handovers happen include between working shifts, clinical settings, different healthcare institutions, and various health professions. Inadequate clinical handovers occur when communication between providers breaks down. Inadequate clinical handovers impart a central issue within health services as the Joint Commission found that 80% of all adverse patient outcomes originate from inadequate handovers. Even more telling, the Commission reports that only 8% of medical schools in a didactic session teach proper patient transfer. Current assessments place the number of handovers per year at approximately 300 million in the United States, 40 million in Australia, and 100 million in the United Kingdom. With these statistics in mind, it becomes ever more apparent the significance communication plays within the current and future of healthcare.

THE CAUSES FOR INADEQUATE HANDOVERS IN HEALTHCARE
Inadequate clinical handovers are mainly preventable barriers to adequate healthcare delivery and can occur in various settings such as within the same hospital or healthcare facility but different departments or levels of care. It can also occur when different facilities are unable to communicate effectively. Various factors contribute to inadequate handovers; however, the main cause lies in the organization of a health facility. Some of these various factors consist of:
- incomplete review of records or assessment procedures
- inadequate handwriting
- overuse of abbreviations
- no support for open communication between providers
In a 2019 systematic review, researchers examined 263 studies and found miscommunication as the main obstacle to clinical handover. Poor communication between providers severely limits the transmission of critical information. When vital information is lost, patients’ health suffers. The National Safety and Quality Health Service (NSQHS) Standards partnered with the Australian Commission describe some of the effects of inadequate handover being “unnecessary delays in diagnosis, treatment, and care; repeated tests, missed or delayed communication of test results; and incorrect treatment or medication errors.” In sum, miscommunication impairs the process of health care services. Furthermore, the NSQHS finds that verbal communication without any documentation relies mostly on memory and categorizes such an exchange as high risk. From this, the extent to which inadequate clinical handover occurs reveals a need to document and transfer sensitive information effectively. It also points to how a standardized protocol is necessary to improve the process.
TOWARDS PROGRESS IN CLINICAL HANDOVERS
The path to improving the clinical handover process remains a blank canvas. In a review study (2011), researchers identified three areas for handover practice. They found targeting management information systems, personal responsibility and accountability, and facilitators of the handover process (leadership and support) can improve patient outcomes immensely. In addition, designing education for clinical handovers remains a promising technique for improving the process. Researchers explain how doctors believe interactive learning styles like simulation or role-play are impactful to learning clinical handover. Even more convincing, they point out the value of feedback and debriefing after each training session.
Healthcare facilities must prioritize communication services within their organizations to improve the clinical handover process. By incorporating standardized protocols that optimize communication efforts, the rate at which medical errors due to inadequate handovers will dampen. For example, optimization techniques for communication efforts include systems management of patient records that allow health providers and patients reliable and frequent access. The future of healthcare services relies on its ability to minimize patients’ risks and predicates the necessity of health communication technology.